- CONTACT INFORMATION
- 806-378-6300
- 806-378-6306
-
Office Hours:
Monday – Thursday
7:30 am – 6:00 pm -
Main Office:
1000 Martin Rd
Amarillo, TX 79107 -
Clinic:
850 Martin Rd
Amarillo, TX 79107
Communicable Disease information
The Communicable Disease department at Amarillo Public Health monitors and reports communicable diseases of concern in Potter and Randall County including flu, RSV, COVID-19, food borne illness (salmonella and others), water borne illness (Campylobacter and others), vaccine preventable diseases (Varicella, measles and others), hospital acquired illnesses, animal bites and other emerging acute and infectious diseases (Mpox and others). The communicable disease team also provides education to the community regarding communicable diseases.
Public Health Communicable Disease Contact Information
- Email: shannon.gregory@amarillo.gov
- Phone: 806-378-6321
- Fax: 806-378-6306
- Office Hours & Location: Monday – Thursday, 7:30 am – 6:00 pm | 1000 Martin Road, Amarillo, TX 79107
- 24/7 Provider Reporting for Communicable Diseases: 806-378-6321
Communicable Disease Clinical Services
- Lice Checks — Provides clearance for children to attend school or preschool.
- Rabies Vaccination — Offers pre- and post-exposure rabies vaccinations. Contact the Communicable Disease Department by phone at 806-378-6321 for details.
- Rare Disease Testing — Available when advised by the Amarillo Public Health Authority.
Required Disease Reporting
The Texas Health and Safety Code requires specific information regarding notifiable conditions be reported. Reporting any suspected or laboratory confirmed notifiable conditions is required from:
- Health care providers
- Hospitals
- Laboratories
- Schools
- Head-Start Facilities
- Daycare Facilities
- Long Term or Acute Care Facilities
- Nursing Facilities and Retirement Communities
You can find the current notifiable conditions on the DSHS website:
Communicable Diseases Helpful Links

Public Health Reports
Computer/phone app to view routes, schedules and real-time tracking of transport vehicles.
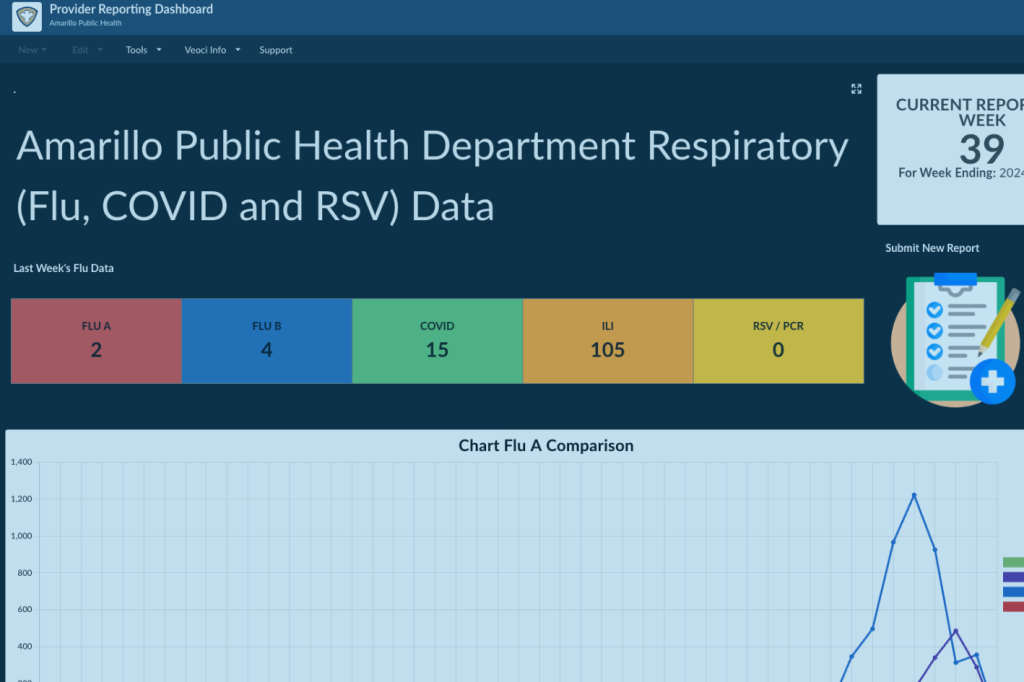
Provider Reporting Dashboard
Providers reporting the flu, COVID-19 and RSV can click here to access the Provider Reporting Dashboard.

Notifiable Condition Online Reporting
Click here to access the online Provider and Stakeholder Notifiable Condition Reporting Form.
Communicable Disease FAQs & assistance
Notifiable Conditions FAQs
Measles is a highly contagious respiratory virus. A measles outbreak is considered a public health emergency and should not be taken lightly. It is one of the most contagious infectious diseases.
How do providers report the flu, COVID-19, RSV, or other respiratory illnesses?
Providers can report flu, COVID-19, and RSV cases online through the Provider Reporting Dashboard.
What are the reporting requirements for notifiable conditions in Texas?
The Texas Health and Safety Code mandates the reporting of suspected or laboratory-confirmed notifiable conditions by health care providers, hospitals, laboratories, schools, daycares, long-term care facilities, and other specified organizations.
How do I report notifiable conditions by fax?
- Download the relevant forms:
- Gather lab results (if available).
- Fax all information, including a coversheet, to 806-378-6306, addressed to Communicable Disease.
Who do I contact for communicable disease questions?
For questions, you can reach the Public Health Communicable Disease team using the following methods:
- Email: shannon.gregory@amarillo.gov
- Phone: 806-378-6321 (24/7 reporting available)
- Fax: 806-378-6306
Office Hours: Monday – Thursday, 7:30 am – 6:00 pm
Location: 1000 Martin Road, Amarillo, TX 79107
Common Questions on Disease Prevention
How can I avoid the flu, COVID, RSV, and other respiratory illnesses?
You can reduce the risk of respiratory infections by getting vaccinated, avoiding close contact with sick individuals, covering your coughs and sneezes with a tissue or your elbow, washing your hands frequently, and staying home if you’re feeling unwell. Return to daily activities only after being fever-free for 24 hours with improving symptoms. For more flu prevention tips, visit the CDC Flu Information Page.
How can I prevent stomach illness?
Good hygiene and food safety practices are key. Wash your hands with soap and water for at least 20 seconds, especially before meals and after using the bathroom. Cook food thoroughly, avoid eating undercooked meats or eggs, wash fruits and vegetables before eating, and avoid consuming raw milk or eggs. Learn more from the CDC Handwashing Guide and Global Hygiene Council.
How can I protect myself from pertussis (whooping cough)?
Vaccination is the most effective prevention method. In addition, avoid contact with infected individuals, cover your mouth when coughing or sneezing, wash your hands frequently, and follow your doctor’s antibiotic prescription if diagnosed with pertussis. More information is available from the CDC Pertussis Guide.
How can I protect myself from West Nile Virus?
Reduce mosquito exposure by avoiding outdoor activities at dawn and dusk, using EPA-registered insect repellent, wearing long sleeves and pants, and eliminating standing water near your home. Visit the CDC West Nile Virus Information Page for more details.
How can I protect my newborn from Hepatitis B?
If you are Hepatitis B positive, ensure your healthcare provider is aware. Your newborn should receive the hepatitis B vaccine and a dose of HBIG within 12 hours of birth to prevent transmission. The Perinatal Hepatitis B Prevention Program provides additional resources to protect your baby.
The Perinatal Hepatitis B Prevention Program is available through Public Health to help prevent the transmission of Hepatitis B from mother to newborn during delivery.
The program manages care for hepatitis B surface antigen (HBsAg) positive pregnant women through delivery and ensures that their newborns receive the necessary immunizations and follow-up testing to protect against the virus.
What should I do if bitten by an animal?
Identify the animal for quarantine or rabies testing, wash the wound thoroughly with soap and water, and seek medical attention as wounds may become infected. Rabies prophylaxis may be necessary. Contact your Local Rabies Control Authority (LRCA) for further guidance. Visit Animal Management & Welfare for more information.
Common Questions on Measles
What is measles?
Measles is a highly contagious respiratory virus. A measles outbreak is considered a public health emergency and should not be taken lightly. It is one of the most contagious infectious diseases.
Who is at the highest risk of contracting measles?
People who have received zero or only one dose of the MMR vaccine are at the highest risk of contracting measles.
Who is at high risk of severe illness and complications from measles?
Infants and children younger than five years old, adults older than 20 years old, pregnant individuals, and those with compromised immune systems.
What does it mean to be protected against measles?
The CDC considers you protected from measles if you have written documentation (records) showing at least one of the following:
You received two doses of a measles-containing vaccine and are:
- A school-aged child (grades K-12).
- An adult in a high-risk setting for measles transmission, such as college students, healthcare workers, and international travelers.
You received one dose of a measles-containing vaccine and are:
- A preschool-aged child.
- An adult who is not in ahigh-risk setting for measles transmission.
A laboratory-confirmed test shows you had measles at some point in your life.
A titer result confirms you are immune to measles.
You were born before 1957.
How do I know if I am vaccinated against measles?
If your provider recorded your vaccinations in the state vaccination system, ImmTrac, the health department may be able to help. However, most adults are not in ImmTrac since it is an “opt-in” system. You can visit your local health department to request a vaccination record free of charge — no appointment necessary. Bring a valid ID. You can also contact your primary care provider to check your vaccination record if they use ImmTrac. Without written documentation of measles vaccination, you are considered unvaccinated.
What does it mean if I am under-vaccinated against measles?
It means you have received only one of the two required doses of the measles vaccine.
If I am immunocompromised, do I need to get revaccinated for measles?
No.
Will I ever need a booster vaccine for measles?
No.
I am an adult and unvaccinated or don’t have documentation of the measles vaccine. Do I need to get vaccinated?
Adults born after 1957 who have not received two doses of MMR or had measles should get vaccinated. This is especially important if you:
- Attend school beyond high school.
- Work or volunteer in a healthcare facility.
- Travel internationally, including on cruise ships.
- Are of childbearing age (and are not currently pregnant).
I am currently pregnant. Should I get the measles vaccine?
No, pregnant individuals should not receive the MMR vaccine. Talk to your OB/GYN for more information on how to protect yourself.
I am currently breastfeeding. Is it safe for me to get the measles vaccine?
Yes, it is safe for breastfeeding individuals to receive the MMR vaccine. Breastfeeding does not interfere with the response to the vaccine, and the baby will not be affected through breast milk.
My child has received one dose of the measles vaccine but is not old enough for the second dose. What should I do?
Follow the recommended vaccination schedule:
- First dose at 12-15 months of age.
- Second dose at 4-6 years of age.
Guidance may change during an outbreak and will be adjusted if necessary.
What should I do if I am unvaccinated and exposed to measles?
Immediately isolate yourself from others. Contact your healthcare provider by phone to arrange testing in a way that minimizes exposure to others. Do not go to your doctor’s office unannounced. Watch for symptoms, which typically develop 7 to 21 days after exposure.
What should I do if I am vaccinated and exposed to measles?
Monitor yourself for measles symptoms for 21 days after exposure.
Can fully vaccinated individuals get measles if exposed?
Yes, though it is rare. About 3 out of 100 people who receive two doses of the measles vaccine may still get measles if exposed. However, fully vaccinated individuals tend to have a milder illness and are less likely to spread the disease.
Who is considered a close contact in regards to measles?
Anyone who has shared the same airspace with an infectious person is considered a close contact.
Anyone in the same room as a suspected case, regardless of time spent, is considered exposed.
Measles can remain in the air and on surfaces for up to two hours after an infectious person has left.
The infectious period is four days before rash onset through four days after rash onset (day of rash onset is day 0).
How long must I be around someone to be considered exposed to measles?
There is no minimum exposure time. However, the longer you are around an infectious person, the greater your chance of becoming infected.
Why do you need to know my close contacts if I have measles?
Post-exposure prophylaxis must be given quickly and within a specific time frame. Identifying close contacts helps protect them from infection.
I just got the measles vaccine and now have a rash. Does this mean I have measles?
- About 10% of individuals who receive the measles vaccine develop a fever and rash about one week after vaccination.
- If you received the measles vaccine 6-45 days before the rash, a positive IgM test does not necessarily mean you have measles.
- A negative IgM test, however, rules out measles.
- If you were vaccinated more than 14 days before illness onset, a viral specimen should be collected to confirm the rash is due to measles.
- Testing is not recommended for those vaccinated 6-14 days prior to rash onset unless they were exposed to a confirmed case.
Can I get measles from someone who just got the measles vaccine?
No. Vaccine virus transmission does not occur from a vaccinated person, even in those who develop a rash. Person-to-person transmission of the vaccine virus has never been documented.
What are the exclusion criteria for my child’s school if they test positive for or are exposed to measles?
There are multiple exclusion scenarios:
- Confirmed measles case: The individual must stay home and avoid public places until four days after the rash begins and they are well enough to return.
- Unvaccinated individuals: If they receive one dose of the MMR vaccine within 72 hours of exposure, they can return immediately. A second dose is required 28 days later. If they do not get vaccinated within 72 hours, they must isolate at home for 21 days.
- Unvaccinated individuals refusing the MMR vaccine: Must stay home for 21 days after exposure. If exposed to multiple cases, the exclusion period extends.
- Individuals with one dose of MMR: A second dose should be given immediately if 28 days have passed since the first dose. No additional quarantine is required.
- Fully vaccinated individuals: Should monitor for symptoms for 21 days after exposure.
The Texas Administrative Code (TAC) Rule §97.7 requires schools to exclude all exposed students without documentation of two measles vaccine doses or proof of immunity for at least 21 days after the last exposure.
How contagious is measles?
Measles is highly contagious and spreads through the air when an infected person coughs or sneezes. If one person has measles, 9 out of 10 unvaccinated people around them will also become infected.
What are the complications of measles?
Common complications include diarrhea and ear infections. Severe complications include pneumonia, encephalitis (brain swelling), hospitalization, pregnancy complications, and even death.
What cleaning protocols help prevent measles spread?
Routine cleaning of hard surfaces with a viricidal cleaner is recommended, especially during flu, RSV, and COVID seasons. If a measles case is suspected, avoid entering the space for at least two hours after the infected person has left.
